Using a novel imaging technique, researchers followed in real time the movement of immune cells in a live mouse and identified a key factor responsible for triggering inflammatory arthritis.
The study, “Complement C5a receptor is the key initiator of neutrophil adhesion igniting immune complex–induced arthritis,” was published in the journal Science Immunology.
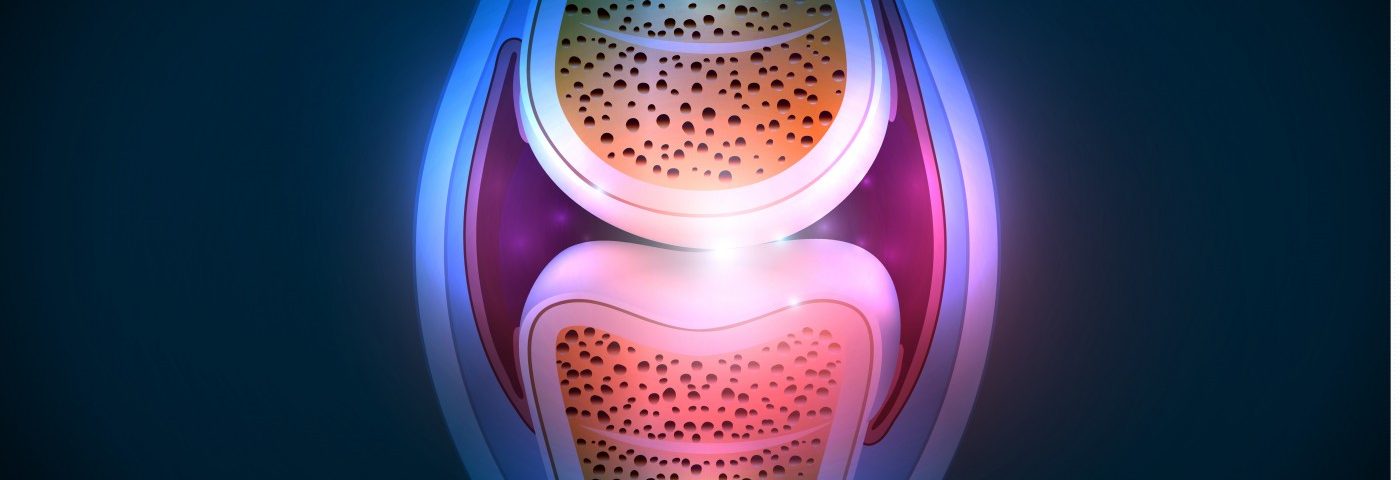
“Inflammatory arthritis is caused when immune cells are recruited from the blood into the joint in a highly regulated process controlled by chemoattractants and adhesion receptors,” Andrew Luster, MD, PhD, chief of the Massachusetts General Hospital (MGH) Division of Rheumatology, Allergy and Immunology, director of MGH’s Center for Immunology and Inflammatory Diseases (CIID), and the study’s lead author, said in a press release.
This type of inflammation is called type III hypersensitivity, and researchers believe it is triggered when immune cells, which are embedded in our tissues, sense what are known as immune complexes (ICs). ICs are antibodies bound to their antigens, setting off an inflammatory response that promotes the recruitment of immune cells — specifically, neutrophils.
“But when the disease has become symptomatic, it is difficult to determine the initial steps that set off the recruitment of immune cells into the joint and the specific roles of the different chemoattractants. Our study was designed to more fully understand this process,” Luster said.
To understand the mechanism that triggers and sets off the attraction of neutrophils, the team of researchers at MGH’s CIID used an imaging technique to follow processes in a living animal. Called multiphoton intravital microscopy, the technology allowed researchers to follow in real time the development of IC-induced inflammatory arthritis in mice.
The team found that a specific receptor called complement C5a receptor (C5aR) was the key protein triggering neutrophil adhesion to the endothelial cells in the joint, setting off inflammation.
Once neutrophils reach the joint space, they initiate a signaling cascade that leads to the release of chemokines by cells lining the joint, which in turn amplifies the infiltration of the immune cells and their movement into the joint space.
“The control of immune cell entry into the joint represents a major point at which new therapies could be developed to reduce the symptoms of inflammatory arthritis,” said Luster, who is also the Harrison Professor of Medicine at Harvard Medical School.
“Imaging of the joint could help evaluate the mechanism of a drug’s therapeutic effect, and if a process turns out to be mediated by more than one chemoattractant, understanding the mechanism would allow the rational design of combination therapies to completely shut down critical steps in the process,” he said.
In the future, the team plans to better understand the characteristics of the cells in the joints that support the key role of C5a in initiating type III hypersensitivity inflammation.