Researchers at the University of Birmingham in England unraveled the key role of different types of fibroblasts — cells that synthesize extracellular matrix and collagen — in rheumatoid arthritis (RA).
The study, “Rheumatoid synovial fibroblasts differentiate into distinct subsets in the presence of cytokines and cartilage,” was published in the journal Arthritis Research and Therapy.
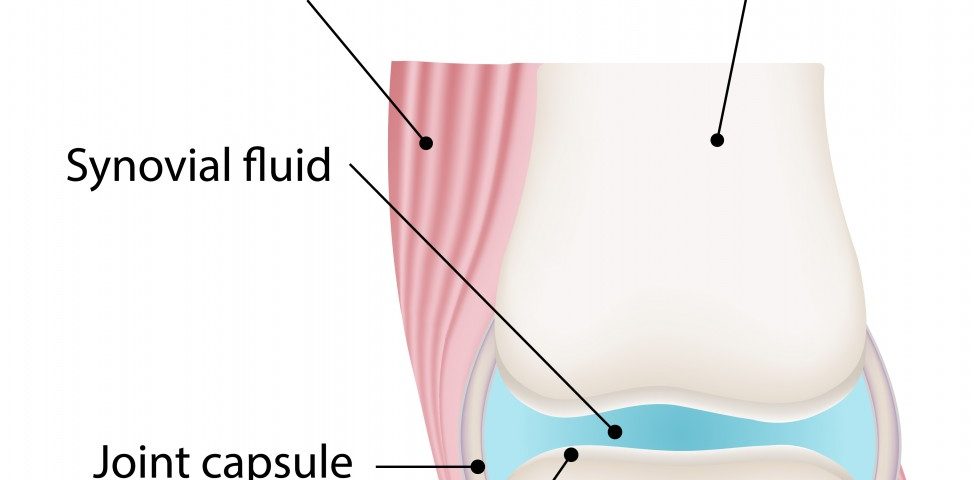
Specific synovial fibroblasts are located at the synovial membrane (also known as the synovium), a specialized connective tissue that lines the inner surface of human joints.
In this study, researchers at the University of Birmingham’s Institute of Inflammation and Aging identified two types of synovial fibroblasts, defined by the expression of different markers at the cells’ surface, namely PDPN and CD248.
The team investigated the role of each type of synovial fibroblasts in RA by growing these fibroblasts from RA patients in vitro within an artificial synovium, then activating them through exposure to small signaling molecules called cytokines. The artificial synovium was then inserted into mice, where researchers were able to analyze the role of synovial fibroblasts.
When looking at the implanted artificial synovium, researchers observed that the inner layer, located closest to the cartilage, was populated by invasive PDPN-synovial fibroblasts; but the noninvasive CD248-synovial fibroblasts were located farther away from the cartilage.
Researchers also observed that “activated” synovial fibroblasts have migration abilities and can travel through blood vessels, reaching other cartilage in the body and causing damage. This ties in with recent findings from other studies.
These results open a potential new avenue for RA therapies by targeting specific types of synovial fibroblasts.
“This study not only shows the existence of distinct sub-sets of synovial fibroblasts, but also suggests that these cells are able to self-organize into lining and sub-lining layers in the presence of cartilage,” Dr. Adam Croft from the University of Birmingham, and the study’s lead author, said in a press release.
“Combined with the difference in migration rates between the two types of cell, these results are extremely promising in terms of finding new therapeutic targets for treatment of rheumatoid arthritis,” he said.
“As PDPN-expressing cells are associated with early fibroblast migration and cartilage erosion in vivo, we propose that PDPN-expressing cells may be an attractive therapeutic target in RA,” the research team wrote in its report.